| Overview Thyroid nodules are solid or fluid-filled lumps that form within thyroid, a small gland located at the base of neck, just above breastbone. Symptom Most thyroid nodules don't cause signs or symptoms. But occasionally some nodules become so large that they can be felt, be seen, be seen, often as a swelling at the base of your neck, press on windpipe or esophagus, causing shortness of breath or difficulty swallowing. In some cases, thyroid nodules produce additional thyroxine, a hormone secreted by thyroid gland. The extra thyroxine can cause symptoms of an overproduction of thyroid hormones (hyperthyroidism), such as: unexplained weight loss, increased sweating, tremor, nervousness, rapid or irregular heartbeat. Only a small number of thyroid nodules are cancerous. But determining which nodules are cancerous can't be done by evaluating symptoms alone. Most cancerous thyroid nodules are slow growing and may be small when the doctor discovers them. Aggressive thyroid cancers are rare with nodules that may be large, firm, fixed and rapid growing. | 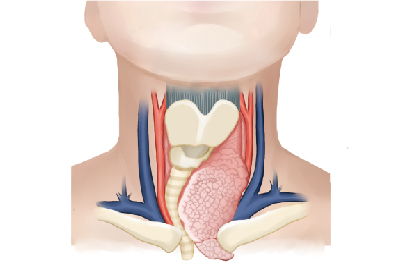 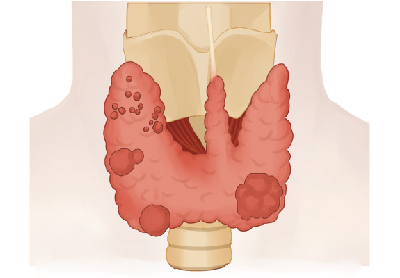 |
Treatment
Although surgery remains the gold standard for treating symptomatic benign and/or malignant thyroid nodules, radiofrequency ablation (RFA) has emerged as a minimally invasive treatment option for high risk patients and those who decline surgery.
For benign nodules, when compared to observation alone, thyroid nodules treated with RFA significantly decreased in volume with improvement in symptom scores at the 6-month follow-up visit (1,2,3). A retrospective study comparing patients treated with thyroidectomy versus those treated with RFA found that patients who underwent surgery had higher postoperative complications (6% vs. 1%, P=0.02) and needed longer hospitalization (6.6±1.6 vs. 2.1±0.9 days, P<0.01) (4). These findings are supported by a meta-analysis which also showed comparable symptom improvement in patients treated with thyroidectomy or RFA, but found that those who underwent RFA had lower incidences of hoarseness, hypothyroidism, pain, and hospitalization time (5).
A prospective study by Zhang et al. (6) found that of 98 PTMC ablated, 10.2% completely resolved within 6 months (median follow-up of 7.8 months) without evidence of short-term recurrence or metastatic lymph node development. This was supported by Lim et al. (7) who looked at 152 PTMCs over a mean follow-up period of 39 months and found complete disappearances in 91.4% of RFA ablated tumors with an overall complication rate of 3%. A subsequent sub-analysis on this same cohort of patients with more than 5-year follow-up found a complete disappearance rate of 100% at the 60-month follow-up with a complication rate of 1.4% (8).
RFA for treating local recurrence in WDTC was first described by Dupuy et al. (9) in 2001 as a small case series of eight patients. With a mean follow-up of 10.2 months, six patients had no evidence of tumor after RFA treatment on US and/or repeat FNA. Subsequent studies found RFA sessions caused disappearance and/or significant volume reduction of metastatic lymph node deposits as well as decrease in serum thyroglobulin levels at last follow-up (10,11,12). Specifically, Kim et al. (11) retrospectively looked at patients with recurrent WDTC less than 2 cm who were treated with RFA or surgery and found comparable 3-year recurrence-free rates at 92.6% and 92.2% respectively. Additionally, a meta-analysis found the pooled proportion of patients with complete disease disappearance after RFA treatment to be 68.8%, the pooled serum thyroglobulin reduction of 71.6% and the complication rate of 5.8% (13).
Reference List
1. Deandrea M, Sung JY, Limone P, et al. Efficacy and Safety of Radiofrequency Ablation Versus Observation for Nonfunctioning Benign Thyroid Nodules: A Randomized Controlled International Collaborative Trial. Thyroid 2015;25:890-6.
2. Baek JH, Kim YS, Lee D, et al. Benign predominantly solid thyroid nodules: prospective study of efficacy of sonographically guided radiofrequency ablation versus control condition. AJR Am J Roentgenol 2010;194:1137-42.
3. Cesareo R, Pasqualini V, Simeoni C, et al. Prospective study of effectiveness of ultrasound-guided radiofrequency ablation versus control group in patients affected by benign thyroid nodules. J Clin Endocrinol Metab 2015;100:460-6.
4. Che Y, Jin S, Shi C, et al. Treatment of Benign Thyroid Nodules: Comparison of Surgery with Radiofrequency Ablation. AJNR Am J Neuroradiol 2015;36:1321-5.
5. Guan SH, Wang H, Teng DK. Comparison of ultrasound-guided thermal ablation and conventional thyroidectomy for benign thyroid nodules: a systematic review and meta-analysis. Int J Hyperthermia 2020;37:442-9.
6. Zhang M, Luo Y, Zhang Y, et al. Efficacy and Safety of Ultrasound-Guided Radiofrequency Ablation for Treating Low-Risk Papillary Thyroid Microcarcinoma: A Prospective Study. Thyroid 2016;26:1581-7.
7. Lim HK, Cho SJ, Baek JH, et al. US-Guided Radiofrequency Ablation for Low-Risk Papillary Thyroid Microcarcinoma: Efficacy and Safety in a Large Population. Korean J Radiol 2019;20:1653-61.
8. Cho SJ, Baek SM, Lim HK, et al. Long-Term Follow-Up Results of Ultrasound-Guided Radiofrequency Ablation for Low-Risk Papillary Thyroid Microcarcinoma: More Than 5-Year Follow-Up for 84 Tumors. Thyroid 2020;30:1745-51.
9. Dupuy DE, Monchik JM, Decrea C, et al. Radiofrequency ablation of regional recurrence from well-differentiated thyroid malignancy. Surgery 2001;130:971-7.
10. Baek JH, Kim YS, Sung JY, et al. Locoregional control of metastatic well-differentiated thyroid cancer by ultrasound-guided radiofrequency ablation. AJR Am J Roentgenol 2011;197:W331-6.
11. Kim JH, Yoo WS, Park YJ, et al. Efficacy and Safety of Radiofrequency Ablation for Treatment of Locally Recurrent Thyroid Cancers Smaller than 2 cm. Radiology 2015;276:909-18.
12. Lee SJ, Jung SL, Kim BS, et al. Radiofrequency ablation to treat loco-regional recurrence of well-differentiated thyroid carcinoma. Korean J Radiol 2014;15:817-26.13. Suh CH, Baek JH, Choi YJ, et al. Efficacy and Safety of Radiofrequency and Ethanol Ablation for Treating Locally Recurrent Thyroid Cancer: A Systematic Review and Meta-Analysis. Thyroid 2016;26:420-8.